Link: https://checkyourwork.kelleykga.com/p/cdc-downplayed-news-of-vax-myocarditis
Graphic:
Excerpt:
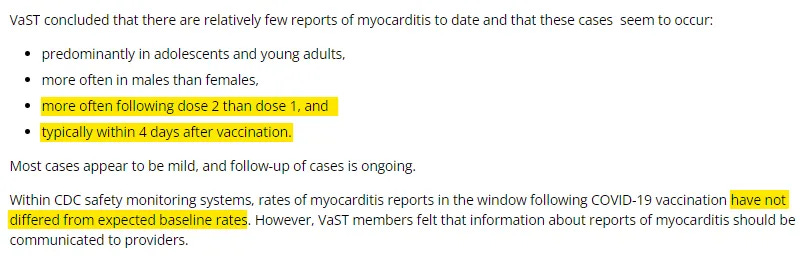
With the recent discovery that the CDC drafted — but never sent — a Health Alert in May 2021 about myocarditis after mRNA vaccination, I put together this timeline about vaccine myocarditis news and updates from government officials. I include a combination of documents from CDC and FDA, as well as what was covered in the mainstream media.
I think this timeline shows a pattern in which CDC & FDA failed to adequately investigate and inform the public about the risks of myocarditis early in the vaccine rollout. However, there was public acknowledgement by the CDC, as early as May 20, 2021, about a potential pattern of myocarditis after the 2nd dose of mRNA vaccines, particularly in young men.
On June 1, 2021, the CDC confirmed that they had identified a higher than expected signal of myocarditis for young men after mRNA vaccination, but that they still recommended Covid vaccination for everyone in this age group. Despite a lot more analysis and discussion of myocarditis after that, and a changing landscape with widespread natural immunity, the CDC & FDA position has changed very little since that time.
Author(s): Kelley in Georgia
Publication Date: 19 Jan 2024
Publication Site: Check your Work on substack