Link: https://jamanetwork.com/journals/jamaoncology/article-abstract/2821594
Excerpt:
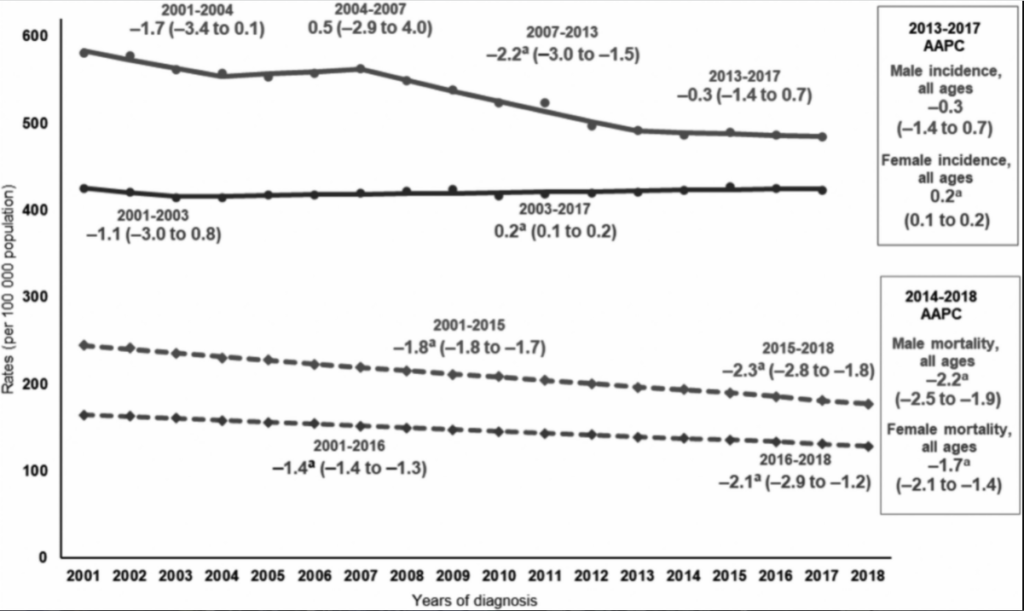
Importance Half of all carriers of inherited cancer-predisposing variants in BRCA1 and BRCA2 are male, but the implications for their health are underrecognized compared to female individuals. Germline variants in BRCA1 and BRCA2 (also known as pathogenic or likely pathogenic variants, referred to here as BRCA1/2 PVs) are well known to significantly increase the risk of breast and ovarian cancers in female carriers, and knowledge of BRCA1/2 PVs informs established cancer screening and options for risk reduction. While risks to male carriers of BRCA1/2 PVs are less characterized, there is convincing evidence of increased risk for prostate cancer, pancreatic cancer, and breast cancer in males. There has also been a rapid expansion of US Food and Drug Administration–approved targeted cancer therapies, including poly ADP ribose polymerase (PARP) inhibitors, for breast, pancreatic, and prostate cancers associated with BRCA1/2 PVs.
Observations This narrative review summarized the data that inform cancer risks, targeted cancer therapy options, and guidelines for early cancer detection. It also highlighted areas of emerging research and clinical trial opportunities for male BRCA1/2 PV carriers. These developments, along with the continued relevance to family cancer risk and reproductive options, have informed changes to guideline recommendations for genetic testing and strengthened the case for increased genetic testing for males.
Conclusions and Relevance Despite increasing clinical actionability for male carriers of BRCA1/2 PVs, far fewer males than female individuals undergo cancer genetic testing. Oncologists, internists, and primary care clinicians should be vigilant about offering appropriate genetic testing to males. Identifying more male carriers of BRCA1/2 PVs will maximize opportunities for cancer early detection, targeted risk management, and cancer treatment for males, along with facilitating opportunities for risk reduction and prevention in their family members, thereby decreasing the burden of hereditary cancer.
Author(s): Heather H. Cheng, MD, PhD1,2; Jeffrey W. Shevach, MD3; Elena Castro, MD, PhD4; et al
JAMA Oncol. 2024;10(9):1272-1281.
doi:10.1001/jamaoncol.2024.2185
Publication Date: July 25, 2024
Publication Site: JAMA Oncology