Excerpt:
Although the regional hospital in the city of Orangeburg delivers babies, the birth outcomes in the county are awful by any standard. In 2021, nearly 3% of all Black infants in Orangeburg County died before their 1st birthday.
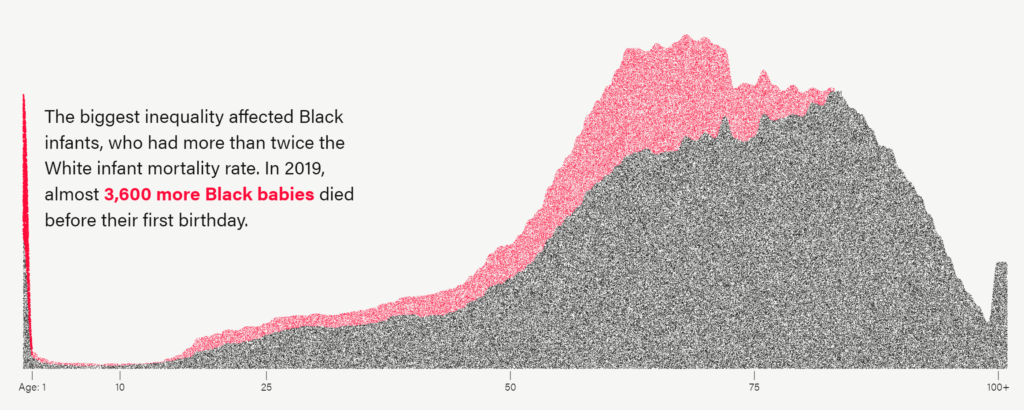
Nationally, the average is about 1% for Black infants and less than 0.5% for white infants.
Meanwhile, Orangeburg County’s infant mortality rate for babies of all races is the highest in South Carolina, according to the latest data published by the South Carolina Department of Health and Environmental Control.
By 2030, the federal government wants infant mortality to fall to 5 or fewer deaths per 1,000 live births. According to annual data compiled by the Centers for Disease Control and Prevention, 16 states have already met or surpassed that goal, including Nevada, New York, and California. But none of those states are in the South, where infant mortality is by far the highest in the country, with Mississippi’s rate of 8.12 deaths per 1,000 live births ranking worst.
Even in those few Southern states where infant mortality rates are inching closer to the national average, the gap between death rates of Black and white babies is vast. In Florida and North Carolina, for example, the Black infant mortality rate is more than twice as high as it is for white babies. A new study published in JAMA found that over two decades Black people in the U.S. experienced more than 1.6 million excess deaths and 80 million years of life lost because of increased mortality risk relative to white Americans. The study also found that infants and older Black Americans bear the brunt of excess deaths and years lost.
….
The state Department of Health and Human Services — which administers Medicaid, the health coverage program for low-income residents, and pays for more than half of all births in South Carolina — claims accidental deaths were the No. 1 reason babies covered by Medicaid died from 2016 to 2020, according to Medicaid spokesperson Jeff Leieritz.
But the state health department, where all infant death data is housed, reported birth defects as the top cause for the past several years. Accidental deaths ranked fifth among all causes in 2021, according to the 2021 health department report. All but one of those accidental infant deaths were attributed to suffocation or strangulation in bed.
Author(s): Lauren Sausser
Publication Date: 22 May 2023
Publication Site: Kaiser Health News