Graphic:
Excerpt:
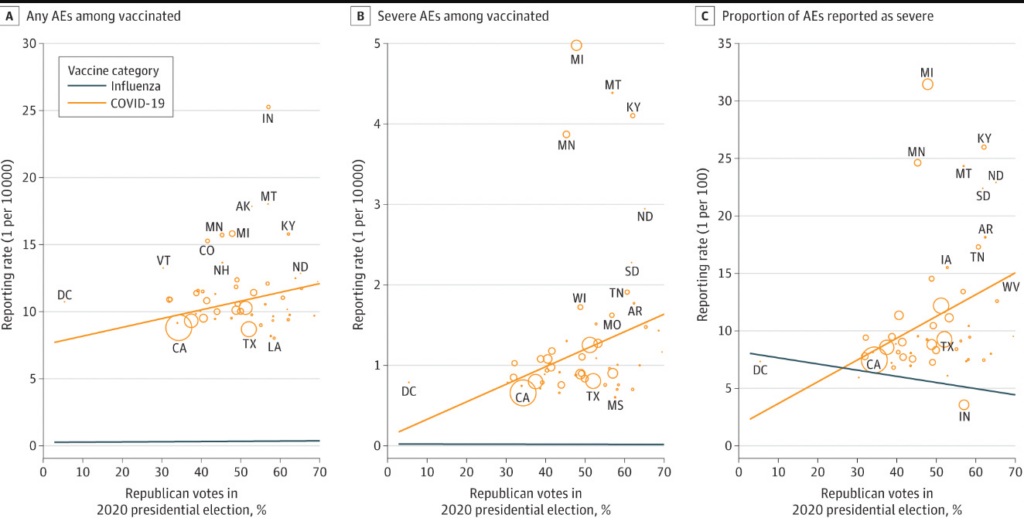
Now let’s turn to the paper. Here is what the authors find (weak correlation btw voting and vaccine injuries) , and here are the issues.
- These data are ecological. It doesn’t prove that republicans themselves are more likely to report vaccine injuries. It would not be difficult to pair voting records with vaccine records at an individual patient level if the authors wished to do it right— another example of research laziness.
- What if republicans actually DO have more vaccine injuries? The authors try to correct for the fact by adjusting for influenza adverse events.
Let me explain why this is a poor choice. The factors that predict whether someone has an adverse event to influenza vaccine may not be the same as those that predict adverse events from covid shots. It could be that there are actually more covid vaccine injuries in one group than another— even though both had equal rates of influenza injuries.
Another way to think of it is, there can be two groups of people and you can balance them by the rate with which they get headaches from drinking wine, but one group can be more likely to get headaches from reading without glasses because more people in that group wear glasses. In other words, states with more republicans might be states with specific co-morbidities that predict COVID vaccine adverse side effects but not influenza vaccine side effects. We already know that COVID vaccine injuries do affect different groups (young men, for e.g.).
Author(s): Vinay Prasad
Publication Date: 2 Apr 2024
Publication Site: Vinay Prasad’s Thoughts and Observations at substack