Link:https://www.kidney.org/news/covid-19-and-its-impact-kidney-patients-utilizing-u-s-dialysis-centers
Excerpt:
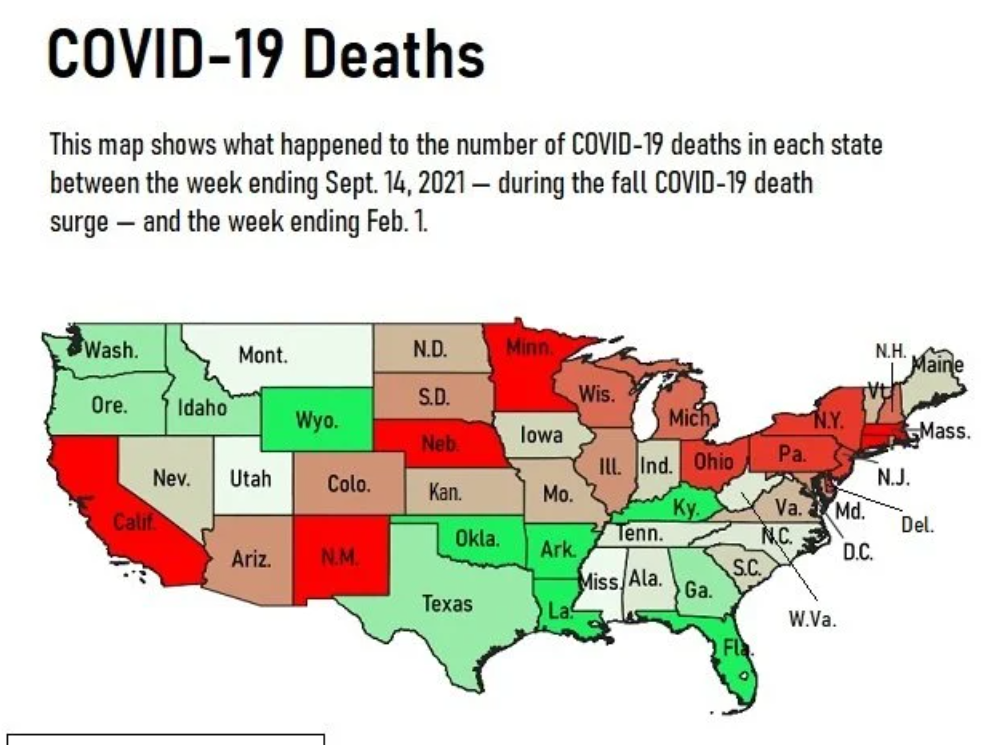
The National Kidney Foundation (NKF) and the American Society of Nephrology (ASN) stress the precarious position people with kidney failure, who are immunocompromised, face as the recent Omicron wave continues to spread among patients and staff at dialysis facilities. Cases of COVID-19 are causing serious illness, forcing shortened treatment times for patients, and exacerbating shortages in staff and supplies that impede access to this life-sustaining treatment. COVID-19’s impact on people with kidney diseases has resulted in the first decline in the number of patients on dialysis in the United States in the 50-year history of the Medicare ESRD Program.
…..
There are 783,000 individuals in the United States who have kidney failure, and just under 500,000 of these individuals require life-sustaining dialysis delivered in a dialysis center three times a week, four hours a day. During dialysis treatments, patients typically sit near other patients and staff in facilities that are not always well ventilated. Many of these patients are older, low-income, and from historically disadvantaged communities, and most have underlying conditions like diabetes and cardiovascular diseases.
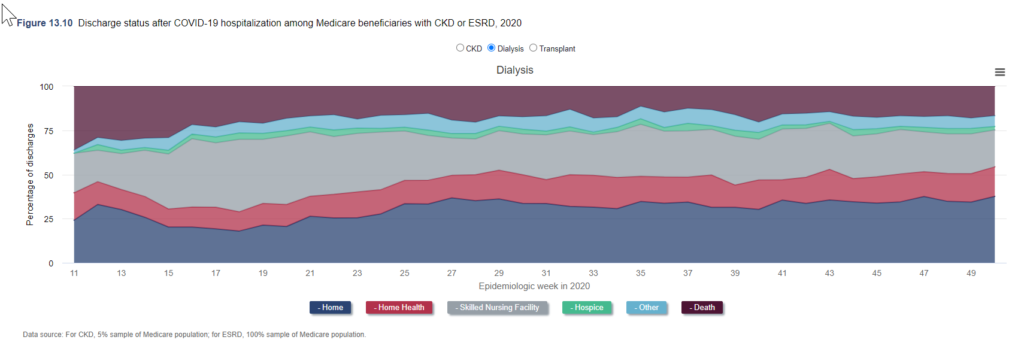
Despite concerted efforts by dialysis organizations, nephrologists, and other clinicians to slow its spread, COVID-19 continues to run rampant through dialysis facilities. According to data from the US Renal Data System, 15.8% of all patients on dialysis in the United States had contracted COVID-19 as of the end of 2020. During the winter 2020 wave, weekly deaths due to COVID-19 peaked at nearly 20% and annual mortality during 2020 was 18% higher than in 2019.[1]
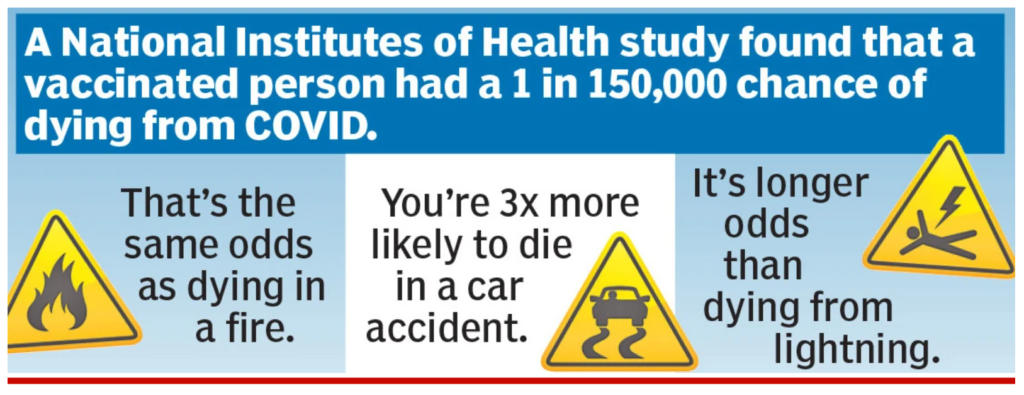
Despite these high rates of infection and mortality, dialysis patients were not prioritized for access to immunization when the vaccines became available a year ago even though evidence shows that the immune response to vaccination is blunted in dialysis patients. Furthermore, although antibody levels decline more rapidly in dialysis patients than in the general population[i], dialysis patients were not prioritized by the Food and Drug Administration (FDA) or the Centers for Disease Control and Prevention (CDC) when third doses of the vaccine were approved in August.[2] In addition, dialysis patients were also excluded from the groups eligible to receive prophylactic long-acting antibody therapy targeting the SARS-CoV-2 virus. Lastly, the National Institutes of Health did not receive funding for COVID-19 research to help people with kidney diseases or failure in any of last year’s relief packages.
[1] https://adr.usrds.org/2021/supplements-covid-19-disparities/13-covid-19-supplement
Publication Date: 18 Jan 2022
Publication Site: National Kidney Foundation