Link:https://allisonschrager.substack.com/p/known-unknowns-27b
Excerpt:
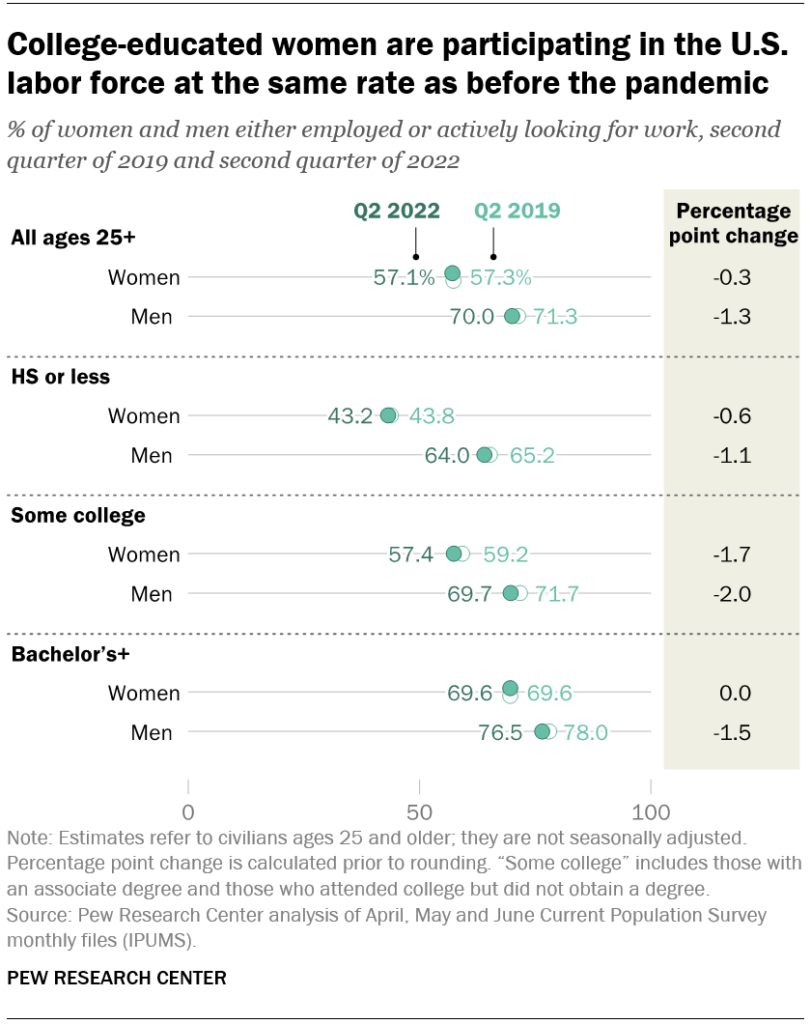
The economy is still short 4.2 million jobs, but as the virus (hopefully) recedes and remaining restrictions are lifted, these trends should continue. The labor market is on the road to recovery—or the cyclical piece of it is, anyway. But during each recession we see many prime-age men leave the labor force and never come back. This was the case during the last recession, too. Prime male labor force participation is still down nearly 1 percentage point from pre-pandemic levels, and this poses huge costs to the economy because a large number of productive workers are simply sitting out. This is terrible for social reasons as well, because work is important to feeling productive, for increasing stability, for marriage, and being fully productive members of society.
This is a difficult economic problem that falls under the category of “structural,” which means that the Fed’s tools are not well-equipped to deal with it. Even with a tight labor market and rising wages, men are simply not working.
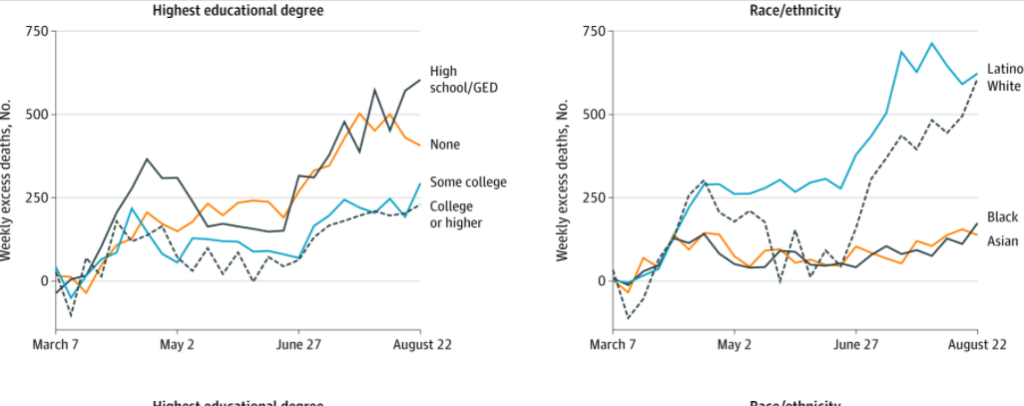
Instead, we need to think more creatively and just fix what’s broken. The common answer is that some of this is driven by a skill mismatch and that there just aren’t many good jobs for men without a college degree. I’m not sure that’s true, it’s very hard to find a good plumber or electrician, which are very well-paying jobs that don’t require a college degree. But they do require skills and training. Community college is often the answer we are given, but it has a terrible track record, primarily because it’s trying to paper over a bigger problem, namely the terrible quality of secondary school, which often fails to properly educate our teenagers. It seems like if we really wanted to keep men from leaving the labor market, this is the low-hanging fruit. Many people drop out of community college, but high school graduation rates are at record highs (or at least they were pre-pandemic). We can raise standards and accountability and fund more vocational high schools. However, tech education has become less popular from the 1980s to 2013, even if the skills are still in quite high demand.
Author(s): Allison Schrager
Publication Date: 7 Feb 2022
Publication Site: Known unknowns