Graphic:
Excerpt:
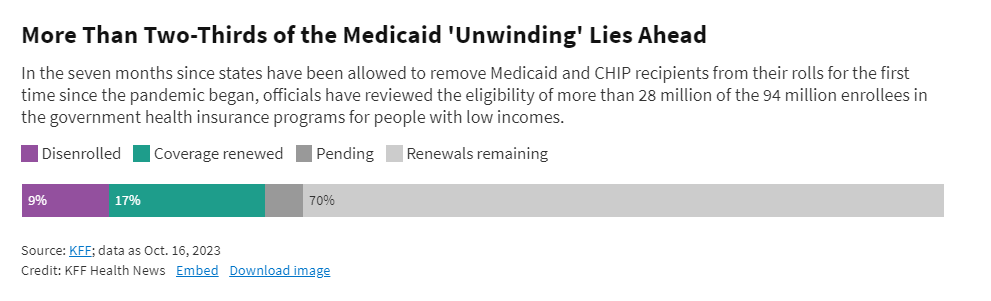
Seven months into what was predicted to be the biggest upheaval in the 58-year history of the government health insurance program for people with low incomes and disabilities, states have reviewed the eligibility of more than 28 million people and terminated coverage for over 10 million of them. Millions more are expected to lose Medicaid in the coming months.
The unprecedented enrollment drop comes after federal protections ended this spring that had prohibited states from removing people from Medicaid during the three pandemic years. Since March 2020, enrollment in Medicaid and the related Children’s Health Insurance Program had surged by more than 22 million to reach 94 million people.
The process of reviewing all recipients’ eligibility has been anything but smooth for many Medicaid enrollees. Some are losing coverage without understanding why. Some are struggling to prove they’re still eligible. Recipients and patient advocates say Medicaid officials sent mandatory renewal forms to outdated addresses, miscalculated income levels, and offered clumsy translations of the documents. Attempting to process the cases of tens of millions of people at the same time also has exacerbated long-standing weaknesses in the bureaucratic system. Some suspect particular states have used the confusing system to discourage enrollment.
Author(s): Phil Galewitz and Katheryn Houghton and Brett Kelman and Samantha Liss
Publication Date: 2 Nov 2023
Publication Site: Kaiser Health News